An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Teaching Clinical Reasoning and Problem-solving Skills Using Human Patient Simulation
Deepti vyas , pharmd, erica j ottis , pharmd, frank j caligiuri , pharmd.
- Author information
- Article notes
- Copyright and License information
Corresponding Author: Deepti Vyas, PharmD, California Northstate College of Pharmacy, Sacramento, CA 95819. Tel: 765-490-7698. E-mail: [email protected]
Received 2011 Feb 1; Accepted 2011 Jul 30.
This paper discusses using human patient simulation (HPS) to expose students to complex dynamic patient cases that require clinical judgment, problem-solving skills, and teamwork skills for success. An example of an HPS exercise used to teach multifaceted clinical concepts in a therapeutics course also is provided.
Keywords: simulation, problem solving, virtual learning, clinical judgment, human patient simulation
INTRODUCTION
The Accreditation Council for Pharmacy Education (ACPE) supports the provision of experiences that augment students’ clinical reasoning and problem-solving skills. 1 While improving students’ clinical reasoning is a goal of all doctor of pharmacy (PharmD) programs, it is still not clear how to: (1) adequately provide experiences that improve students’ clinical reasoning; (2) assess students’ reasoning skills; and (3) use technology to supplement traditional pedagogical learning experiences. Clinical judgment requires compilation, analysis, and synthesis of data to make critical decisions about patient care. It also requires conflict resolution when data are contradictory or do not support a previously generated idea. In practice, to accomplish immediate conflict resolution healthcare providers have to identify alternative solutions to the same problem. In this context, clinical judgment skills must be dynamic and adapt to each new case.
The American Association of Colleges of Pharmacy (AACP) Report of the 2009-2010 Academic Affairs Standing Committee defined problem solving as a high-order thinking skill that is achieved when one has mastered each level of Bloom's taxonomy. 2 Bloom's taxonomy encompasses all facets of learning, which include the cognitive, affective, and psychomotor domains. 3 Of these, the cognitive domain seems to receive the most attention and educators strive to provide didactic experiences that touch on knowledge, comprehension, application, analysis, synthesis, and evaluation.
If well executed, traditional written assessments are able to provide excellent cognitive learning opportunities. However, while written assessments are a good measure of a student's cognitive learning, they do not necessarily reflect student performance in clinical practice. Also, it may be difficult to add visual and sensory elements to a written assessment, which is important for a well-rounded learning experience.
Experiential education sets out to supplement traditional didactic coursework with real life applications within a patient care context. However, students sometimes take on more of an observatory role in experiential settings. 4 Additionally, there is an increased risk for errors if students do not exercise good judgment. Educators also have little influence on the type and variety of patients encountered in the clinical setting. To further promote the development of clinical judgment and problem-solving skills, the pharmacy curriculum needs to provide more hands-on clinical opportunities in a controlled environment prior to students’ advanced pharmacy practice experiences (APPEs). Several active-learning strategies have been identified by ACPE, including laboratory experiences, case studies, and instructional technology, to provide hands-on opportunities to students. However, it is unclear how successful these are in recreating real-life patient care scenarios. 1 Additionally, according to the 2009-2010 AACP report, today's learner appreciates activities that provide opportunities to interact with their peers. 2
Benner and colleagues devised a “thinking-in-action” strategy to teach clinical judgment to nursing students. 5 This approach allows educators to recreate scenarios that make students reason through problems as they would unfold in real life situations. Human patient simulation (HPS) training is a “thinking-in-action” strategy that can serve as a bridge between didactic teaching and experiential training. It puts students in an application-based environment without risking patient safety. In HPS, students must “think on their feet” and use their problem-solving and clinical skills to provide patient care in real time. Educators can build HPS scenarios to hone students’ patient counseling and professional communication skills as well as to teach students to critically think through specific therapeutic concepts. Teaching students to think critically rather than simply applying previously accrued knowledge is a difficult task that educators face. Perry theorized that students progress through intellectual development by consecutive stages beginning with “dualism” and ultimately achieving “commitment in relativism.” 6 This means that while novice students believe that there is a black-and-white answer to every problem, as they progress intellectually they realize that sometimes there is no “right” answer to a problem and a certain ambiguity may exist, especially in the practice of pharmacy. While not explicitly stated, the right answer may simply be the one that can be adequately defended and supported with evidence. This state is usually achieved when students draw upon their accumulated experiences and weigh all possible solutions before selecting a particular answer. HPS training provides students the opportunity to apply knowledge learned in the classroom in situations where clinical judgment and conflict resolution also are imperative to providing optimal patient care. Educators can create simple to complex simulation scenarios that enhance student learning and shift students’ intellect toward “commitment in relativism,” a state where students realize that even the experts sometimes disagree.
HPS has been used to teach technical, clinical, and teamwork skills, and is an important part of the medical and nursing curricula. 7-20 Improvements in clinical decision-making skills and leadership skills when HPS is used also have been reported in the nursing literature. 7-15 In a small study, Steadman and colleagues compared HPS to problem-based learning for teaching medical students the management of acute life-threatening emergencies and found that the simulation group performed significantly better in the final assessment, which consisted of 9 separate acute emergency cases. 16 HPS-based learning was superior in improving students’ critical assessment and management skills.
In the pharmacy literature, the use of HPS has been described as an active-learning tool for teaching pharmacotherapy concepts, advanced cardiac life support skills, and other clinical skills. 21-27 Seybert and colleagues used HPS to teach critical care concepts. The study showed positive changes in a majority of students’ self-perceived ability to solve problems as well as greater student satisfaction with high fidelity simulation than with traditional classroom teaching. 27 Besides improvements in clinical judgment, HPS can provide students the opportunity to professionally interact with their peers and improve their teamwork skills. 10,26
The 2010 decision by ACPE to support the inclusion of simulation training for up to 20% of all introductory pharmacy practice experience (IPPE) hours provides the impetus to solidify the role of simulation in the pharmacy curriculum. 1 In a previous study, the authors of this paper showed that simulation training coupled with direct patient care can provide a suitable learning model for IPPEs. 18
HPS offers educators the opportunity to create complex scenarios that hone specific skills, knowledge, and attitudes in students. As pharmacy educators incorporate more clinical reasoning and problem solving in the curricula, HPS should be a top consideration. In this paper, we describe how to develop an HPS exercise that incorporates both clinical reasoning and teamwork skills. We also provide an example of an HPS exercise that has been described in the literature previously. 18
DEVELOPMENT OF A HUMAN PATIENT SIMULATION EXERCISE
Prior to developing an HPS exercise, the components of the simulation must first be determined and planned by the educator. It is vital to anticipate all variations of the exercise as every student reacts differently to the scenarios. This stage of simulation development requires careful training of all parties, especially in scenarios where there is no single, clear solution. Practice sessions prior to the actual simulation can provide crucial information regarding simulation components. HPS often is divided into 3 components: the case preparation or presimulation, the simulation, and the debriefing period. The presimulation exercise generally is used to orient the students to the simulation room and to instruct them about the goals of the exercise. It also can be used to complete presimulation assessments to ensure the students’ preparedness as well as to present the initial case work-up. The simulation exercise itself needs to be carefully scripted and standardized patient roles need to be outlined to ensure that the individuals in these roles remain in character as students work through the scenario. Immediate feedback can be provided during the simulation when a member of the team (usually a faculty member) calls a timeout to introduce a key learning point. A timeout also can be used to guide the student team if assistance is needed during the simulation. During the simulation, the instructor and other trained observers should take notes and complete checklists. At the end of the simulation, the debriefing period provides a dedicated time for student self-reflection regarding their thought process, students’ reflection about their team's performance, and instructor feedback regarding the team's professional, communication, and clinical skills. To provide students feedback regarding their performance and guide discussion during the debriefing session, the checklist from the observers/instructor can prove to be valuable. The debriefing session also can be used to emphasize and clarify key clinical pearls and to help students cope with any emotional reactions that arise during the simulation.

EXAMPLE OF A SIMULATION SCENARIO
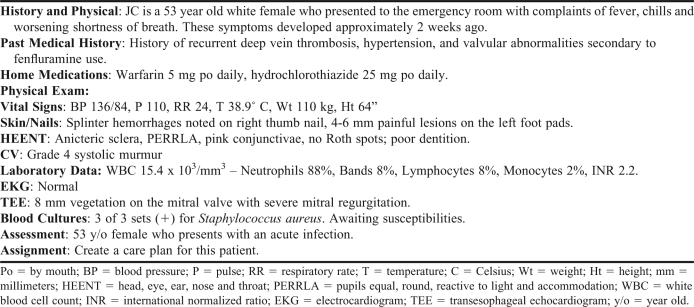
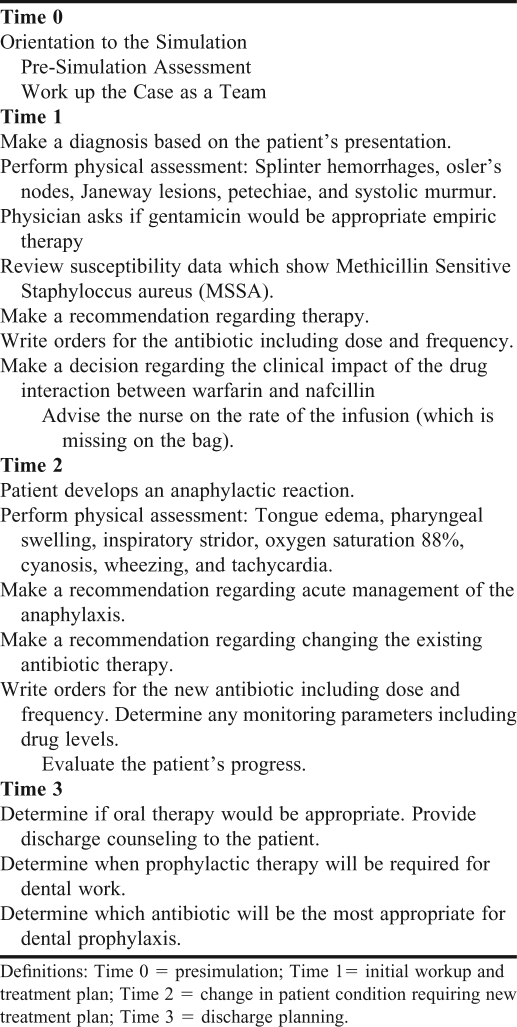
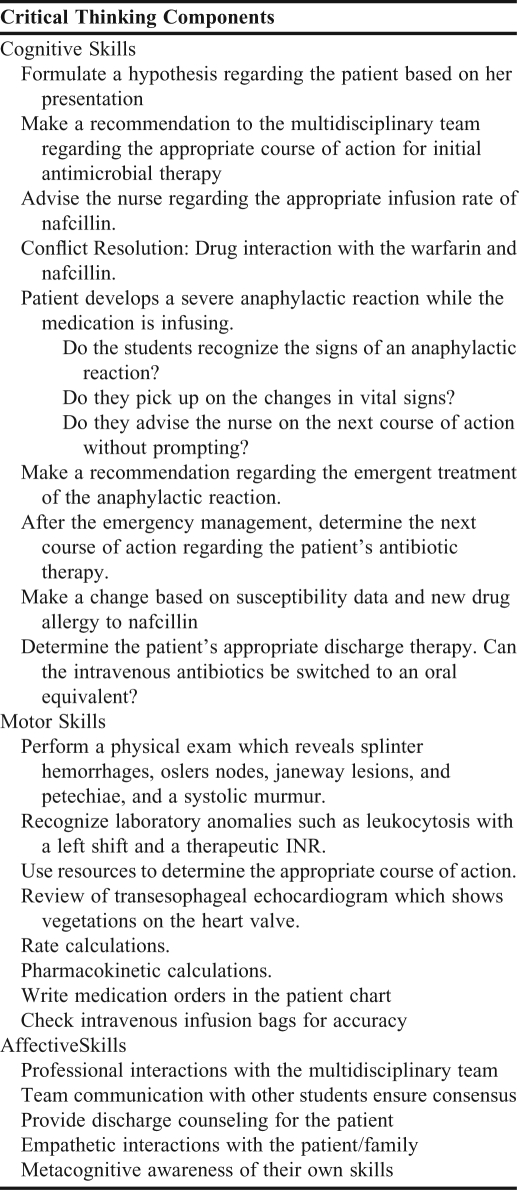
An example of a scenario in which a patient presents to the emergency department with infective endocarditis is described ( Tables 1 and 2 ). The objective of the simulation exercise is to: (1) show students the physiologic changes associated with endocarditis; (2) provide students the opportunity to make decisions regarding first-line therapy, management of an acute emergency, and resolution of the conflict between the drug of choice and the patient's new drug allergy profile, which prevents the students from using the drug of choice. The simulated scenario should be carefully scripted to provide learning opportunities in the various domains of Bloom's taxonomy ( Table 3 ).
Case Information for a Simulation Involving a Patient With Infective Endocarditis
Example of a Scenario in Which Human Patient Simulation Is Used
Components of Bloom's Taxonomy Addressed by a Simulated Patient Case
The scenario may be conducted in a laboratory set up to look like a hospital room with a gurney, high-fidelity mannequin, oxygen tank, and other supplies. To improve the realism of the scenario, a family member played by a standardized patient, a nurse, and a physician should be recruited and trained on the objectives of the exercise and their roles within the scenario. The simulation should consist of a case preparation period, the clinical encounter, and a debriefing period, each 30 minutes in length. Students should be divided into small teams of 2 to 3 for the simulation.
Presimulation (case preparation period). In the presimulation period, each student team should be given the patient's chart with preliminary information ( Table 1 ) and instructed to develop a treatment plan and make antibiotic recommendations to the nurse and physician taking care of the patient.
Clinical encounter . The student team should enter the simulated hospital room, assess the patient, and ask questions. Additionally, the students should professionally interact with the physician and nurse in the room to get relevant information regarding the patient including any laboratory data. At this juncture, the students should have identified an antibiotic regimen based on the preliminary information they received during the presimulation session. Once the nurse administers the chosen antibiotic regimen, the simulated patient should be programmed to develop an anaphylactic reaction in real time. This reaction will not be anticipated and will put students in a stressful situation that requires quick reaction. The students should make recommendations regarding the treatment of the acute emergency and subsequently determine the next course of action regarding the endocarditis therapy. After the acute situation, the students then should be instructed by the physician to provide discharge counseling, especially with regard to antibiotic prophylaxis for dental procedures.
Debriefing. During the debrief session the students should be asked to reflect on their performance during the simulation. This exercise could include a review of each student's strengths and weaknesses during the simulation. The debrief session also should be used to discuss the details of the case and reinforce any clinical pearls that were identified during the simulation exercise. The debriefing also should be an opportunity for students to provide feedback regarding the simulation and areas of improvement.
HPS training provides students the opportunity to practice their skills in a high-stress, low-risk environment. While the educator can effectively bridge the gap between classroom coursework and “real-life” experiences, patient care simulations do not compromise patient safety if the students make an error. Simulation-based training improves students’ knowledge and clinical skills. If used appropriately, simulation training can increase students’ metacognitive awareness which may ultimately shift the student towards a state of “commitment in relativism” as they encounter more complex clinical problems having more than one right answer. Simulation also teaches students to anticipate problems and identify alternate solutions to a problem ahead of the patient encounter. Ideally, this should prepare students for future patient care experiences, which can be dynamic and unpredictable.
- 1. Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. 2006. http://www.acpeaccredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf . Accessed September 22, 2011.
- 2. Oderda GM, Zavod RM, Carter JT, et al. An environmental scan on the status of critical thinking and problem solving skills in colleges/schools of pharmacy: report of the 2009-2010 Academic Affairs Standing Committee. Am J Pharm Educ. 2010;74(10):Article S6. doi: 10.5688/aj7410s6. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Bloom BS, editor. Taxonomy of Educational Objectives. The Classification of Educational Goals. New York, NY: McKay; 1956. Handbook I: Cognitive Domain. [ Google Scholar ]
- 4. Chase P. Rethinking experiential education (or does anyone want a pharmacy student?) Am J Pharm Educ. 2007;71(2):Article 27. doi: 10.5688/aj710227. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Benner P, Stannard D, Hooper PL. A "thinking-in-action" approach to teaching clinical judgment: a classroom innovation for acute care advanced practice nurses. Adv Pract Nurs Q. 1996;1(4):70–77. [ PubMed ] [ Google Scholar ]
- 6. Perry WG. Forms of Intellectual and Ethical Development in the College Years. New York: Henry Holt;; 1970. [ Google Scholar ]
- 7. Baldwin KB. Friday night in the pediatric emergency department: a simulated exercise to promote clinical reasoning in the classroom. Nurs Educ. 2007;32(1):24. doi: 10.1097/00006223-200701000-00008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Henrichs B, Rule A, Grady M, Ellis W. Nurse anesthesia students' perceptions of the anesthesia patient simulator: a qualitative study. Am Assoc Nurs Anesthetists J. 2002;70(3):219. [ PubMed ] [ Google Scholar ]
- 9. Lasater K. High-fidelity simulation and the development of clinical judgment: students' experiences. J Nurs Educ. 2007;46(6):269–276. doi: 10.3928/01484834-20070601-06. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Kyrkjebo JM, Brattebo G, Smith-Strom H. Improving patient safety by using interprofessional simulation training in health professional education. J Interprof Care. 2006;20(5):507–516. doi: 10.1080/13561820600918200. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Henneman EA, Cunningham H. Using clinical simulation to teach patient safety in an acute/critical care nursing course. Nurs Educ. 2005;30(4):172–177. doi: 10.1097/00006223-200507000-00010. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Comer SK. Patient care simulations: role playing to enhance clinical understanding. Nurs Educ Perspect. 2005;26(6):357–361. [ PubMed ] [ Google Scholar ]
- 13. Peteani LA. Enhancing clinical practice and education with high-fidelity human patient simulators. Nurs Educ. 2004;29(1):25–30. doi: 10.1097/00006223-200401000-00008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Feingold CE, Calaluce M, Kallen MA. Computerized patient model and simulated clinical experiences: evaluation with baccalaureate nursing students. J Nurs Educ. 2004;43(4):156–163. doi: 10.3928/01484834-20040401-03. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Spunt D, Foster D, Adams K. Mock code: a clinical simulation module. Nurse Educ. 2004;29(5):192–194. doi: 10.1097/00006223-200409000-00009. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Steadman R.H, Coates WC, Huang YM, Matevosian R, Larmon BR, McCullough L, Ariel D. Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med. 2006;34(1):151–157. doi: 10.1097/01.ccm.0000190619.42013.94. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Lighthall GK, Barr J, Howard SK, et al. Use of fully simulated intensive care unit environment for critical event management training for internal medicine residents. Crit Care Med. 2003;31(10):2437–2443. doi: 10.1097/01.CCM.0000089645.94121.42. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Small SD, Wuerz RC, Simon R, Shapiro N, Conn A, Setnik G. Demonstration of high-fidelity simulation team training for emergency medicine. Acad Emerg Med. 1999;6(4):312–323. doi: 10.1111/j.1553-2712.1999.tb00395.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Marshall RL, Smith JS, Gorman PJ, Krummel TM, Haluck RS, Cooney RN. Use of a human patient simulator in the development of resident trauma management skills. J Trauma. 2001;51(1):17–21. doi: 10.1097/00005373-200107000-00003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Issenberg SB, McGaghie WC, Petrusa ER, Gordon DL, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10–28. doi: 10.1080/01421590500046924. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Tofil NM, Benner KW, Worthington MA, Zinkan L, White ML. Use of simulation to enhance learning in a pediatric elective. Am J Pharm Educ. 2010;74(2):Article 21. doi: 10.5688/aj740221. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Vyas D, Wombwell E, Russell E, Caligiuri F. Creating a hybrid model of introductory pharmacy practice experience: integrating high fidelity simulation and direct patient care. Am J Pharm Educ. 2010;74(9):Article 169. doi: 10.5688/aj7409169. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Mieure KD, Vincent WR, Cox MR, Jones MD. A high-fidelity simulation mannequin to introduce pharmacy students to advanced cardiovascular life support. Am J Pharm Educ. 2010;74(2):Article 22. doi: 10.5688/aj740222. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Seybert AL, Kobulinsky LR, McKaveney TP. Human patient simulation in a pharmacotherapy course. Am J Pharm Educ. 2008;72(2):Article 37. doi: 10.5688/aj720237. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ. 2007;71(3):Article 48. doi: 10.5688/aj710348. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Fernandez R, Parker D, Kalus JS, Miller D, Compton S. Using a human patient simulation mannequin to teach interdisciplinary team skills to pharmacy students. Am J Pharm Educ. 2007;71(3):Article 51. doi: 10.5688/aj710351. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 27. Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Pharmacy student response to patient-simulation mannequins to teach performance-based pharmacotherapeutics. Am J Pharm Educ. 2006;70(3):Article 48. doi: 10.5688/aj700348. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (442.1 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
VIDEO